Tricky Tumors
A brain tumor diagnosis today still represents a death sentence. And death comes quickly. People with a glioblastoma – the most common type of malignant brain tumor – live for another 15 months on average following diagnosis. Patients who have brain metastases from other types of cancer such as breast cancer, lung cancer or melanoma have an average life expectancy of just one year. “For many other types of cancer, treatments have become more targeted and much more successful in the last 10 years,” says Jenny Kienzler, a neurosurgeon at the University Hospital of Lausanne and tumor immunology researcher at UZH.
This isn’t the case with brain tumors. “Today, we’re still using the same standard treatments for many tumors in the brain as we were 20 years ago,” says Kienzler, who is keen to change this. In her research, supported by the UZH Alumni Research Talent Development Fund, she is investigating how brain tumors trick the body’s immune system so they can grow undisturbed. The researcher hopes this will help her find new therapeutic approaches.
Incredibly aggressive
There are several reasons why brain tumors are difficult to treat. One of them is that they are incredibly aggressive. Glioblastoma, for example, can increase the volume of the tumor by more than two cubic centimeters per month. This is why it is usually only discovered once it is already quite large. And it often develops in healthy and comparatively young people, aged around 50 or above – regardless of any risk factors they may have such as smoking, alcohol abuse, obesity or a lack of exercise. Another reason is that brain cancer never really goes away. Even after being removed by surgery and the treatment that follows, the tumor can regrow from sleeper cells that were previously invisible.
And finally, especially in the case of brain tumors, hardly any improvement has been derived from the approach that has truly revolutionized the treatment of other types of cancer in the last ten years: immunotherapy. This treatment uses the body’s own immune system to fight cancer. One particularly successful mechanism has been the so-called checkpoint inhibitors, which prevent the tumor cells of some types of cancer from hijacking the immune system. This is because some tumor cells can interfere with the signaling pathways of the immune system and so effectively disguise themselves to evade it. The checkpoint inhibitors then switch this mechanism off again, causing the immune cells to attack the tumor.
Guardians on the wrong track
However, this type of therapy hardly works at all on tumors in the brain, especially on glioblastoma. First, this is because brain tumor cells resemble the healthy brain cells and so offer hardly any surface for specific drugs to target. Second, the tumor cells create a distinctly immunosuppressive environment. In other words, they weaken the immune system in an even more perfidious way than other types of cancer do.
If the immune system is working, invaders such as pathogens or tumors are systematically destroyed by the defenses. T cells of the immune system are attracted and attack the tumor cells. In a second step, phagocytes, the macrophages, take over and digest the remaining material. But in brain tumors, these macrophages are often reprogrammed. Then not only do they no longer do their job – they also prevent T cells from fighting the tumor cells. This allows the cancer to spread undisturbed. Tumor-associated macrophages like this account for up to 40 percent of the cells in brain tumor tissue, so they play a dominant role.
However, it is not yet known exactly how they are reprogrammed. “Although we know some of the molecules that are involved in the communication between the tumor cells and the macrophages,” says Kienzler, “we still don’t know enough about the actual mechanism itself.” Of course, if researchers were to find out how the reprogramming of the macrophages works, this would also give them approaches for reversing it. What’s more, if such reprogramming were successful in these particularly aggressive tumors, it could probably also be used to treat other types of cancer.
So which macrophage types are reprogrammed by the tumors, and how exactly does this happen? These are the questions Kienzler is trying to answer. First of all, she is in the process of drawing a kind of atlas of the surfaces of the tumor and macrophage cells. This is because communication between different cells takes place via receptors located on their surface. So if the receptors on the tumor and macrophage surfaces are known, this provides clues about the signaling pathways between the cells – and possible ways of blocking them.
Blocking receptors
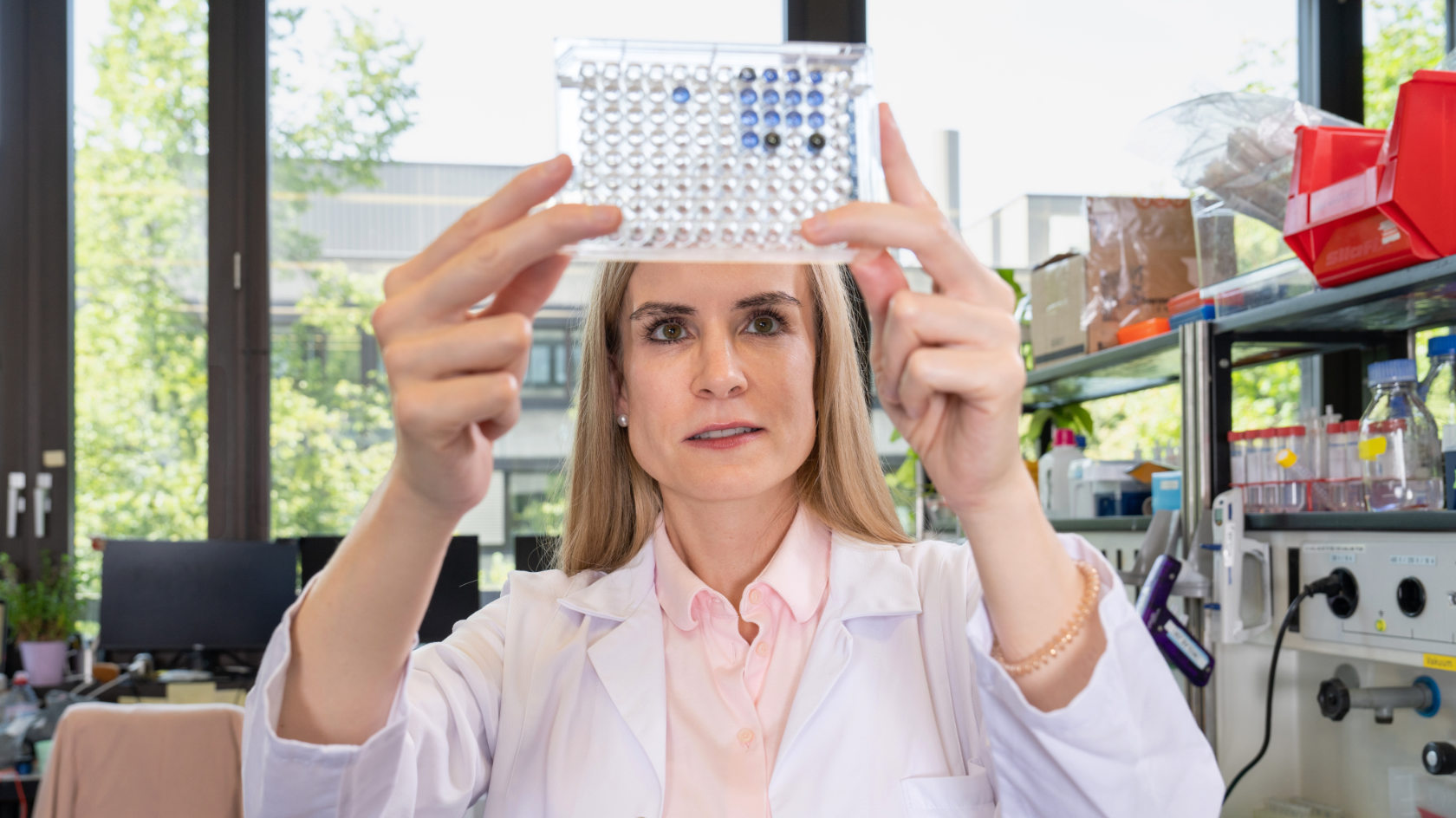
Ideally, Jenny Kienzler wants to identify the receptors that are located on the surface of both the tumor-associated macrophages and the tumor cells. It would then be possible to block these surface markers, as they are referred to in the technical jargon, with a single active ingredient on both cell surfaces. The researcher recently completed this mapping for the most common fatal brain tumor, glioblastoma, using tissue samples from patients. In this tissue, she examined the surface proteins of individual cells using a method called flow cytometry. She identified around 40 markers on the surfaces of macrophage and tumor cells. Roughly 20 of them were present on both cell types. “We were already aware of some of them and knew that they also play a role in other types of cancer,” says Kienzler. Others were previously unknown. “This means we now have a basis to conduct further investigations, which will narrow down to an even greater extent the receptors that could best be targeted using a new therapeutic approach.”
Jenny Kienzler: Operating and doing research
It is rare for someone to divide their working life equally between the clinic and research, as Jenny Kienzler does – at least in Europe. In the USA, in contrast, it is more established and also encouraged for medical clinicians to spend a lot of their time engaged in research. According to Kienzler, this is exactly what is needed to make swifter progress in brain tumor research. “Managing to do both is certainly a challenge,” she says. Both neurosurgery and research are demanding tasks and each of these two roles is more than fulfilling on its own. But Kienzler says that it’s worth striving to do both. The background knowledge of the clinical processes, information about the tumor tissue from the operations and the stories from each patient help her as a researcher.
And because Kienzler treats patients directly and is a neurosurgeon herself, she – unlike other researchers – has easier access to the tumor samples that are needed to conduct the examinations. Conversely, it is generally important for neurosurgeons to be involved in brain tumor research and the development of new therapies as they know the brain and its anatomical structures better than full-time researchers do. The clinicians are absolutely vital, especially for new approaches to treatment such as minimally invasive procedures or innovative therapies used during surgery, because they are the only people who have direct contact with the tumor and so can apply targeted treatments straight away. Jenny Kienzler combines both these roles in one single person.
The neurosurgeon is currently working on using a relatively new method called CITE sequencing to decipher the nucleotide sequence of the RNA of these surface proteins for individual cells. She hopes that this will allow her to identify different cell types with their typical markers, which would provide a clearer basis for new therapies. However, this method is extremely sensitive. Unlike most other methods, it does not work with tumor tissue that is surgically removed from patients and then frozen until the analyses are conducted, but only with freshly removed tissue cells, as Kienzler discovered when she conducted her first experiments. This is because typically 40 to 50 percent of the cells in the brain tumors that have been surgically removed have already died off. “The process of freezing and thawing further destroys the tissue, which then leaves too few intact cells to perform the delicate examinations,” explains Kienzler. The only solution is for freshly removed tumor samples to be transported directly from the operating theater to the lab so the examinations can be done there straight away.
Kienzler is now keen to conduct these analyses, which are currently underway for glioblastoma, for brain metastases as well. Although they look a little different to the tumors in the brain itself, they have a very similar effect on the local immune response and on the macrophages. And here too, there is an urgent need for new therapeutic approaches.
Broad basis for new treatments
Kienzler’s research results can already tell us a little bit about the prognosis for patients. For example, her studies have shown that people with tumor cells that carry a certain type of receptor on the surface survive for less time than other patients. The aim now is to narrow down with greater certainty which markers have which effect, as a basis for developing, among other things, specific antibodies to combat them – creating a new immunotherapy.
In addition to conducting these analyses, the researcher is also taking a closer look at specific tumor-associated messenger substances, known as cytokines. They form part of the signal transmission between cells and regulate cell growth, among other things. As Kienzler has discovered, they also play an important role in attracting the immune system’s macrophages and reprogramming them for the tumor’s benefit. Experiments conducted on mice also revealed that, if the cells are deprived of the ability to produce these kinds of messenger substances, the brain tumors grow at a slower rate. However, it is still unclear exactly how the messenger substances manipulate the macrophages. But what is clear is that these messenger substances also represent a promising potential starting point for a new therapy.