A High-Resolution View of Cancer Cells

Sara Félix, a postdoctoral researcher, sits next to a large grey box, eyes fixed on a monitor. On screen, abstract, green-speckled images appear. But only briefly – seconds later, new and similar images appear. With a click of the mouse, she runs a new measurement. It may not look particularly dramatic, but what’s happening here is a matter of life and death. Inside the grey box is a fully automated fluorescence microscope that can be used to study the factors in tumor cells that make cancers more aggressive. The same microscope can also determine how tumor cells respond to different drugs.
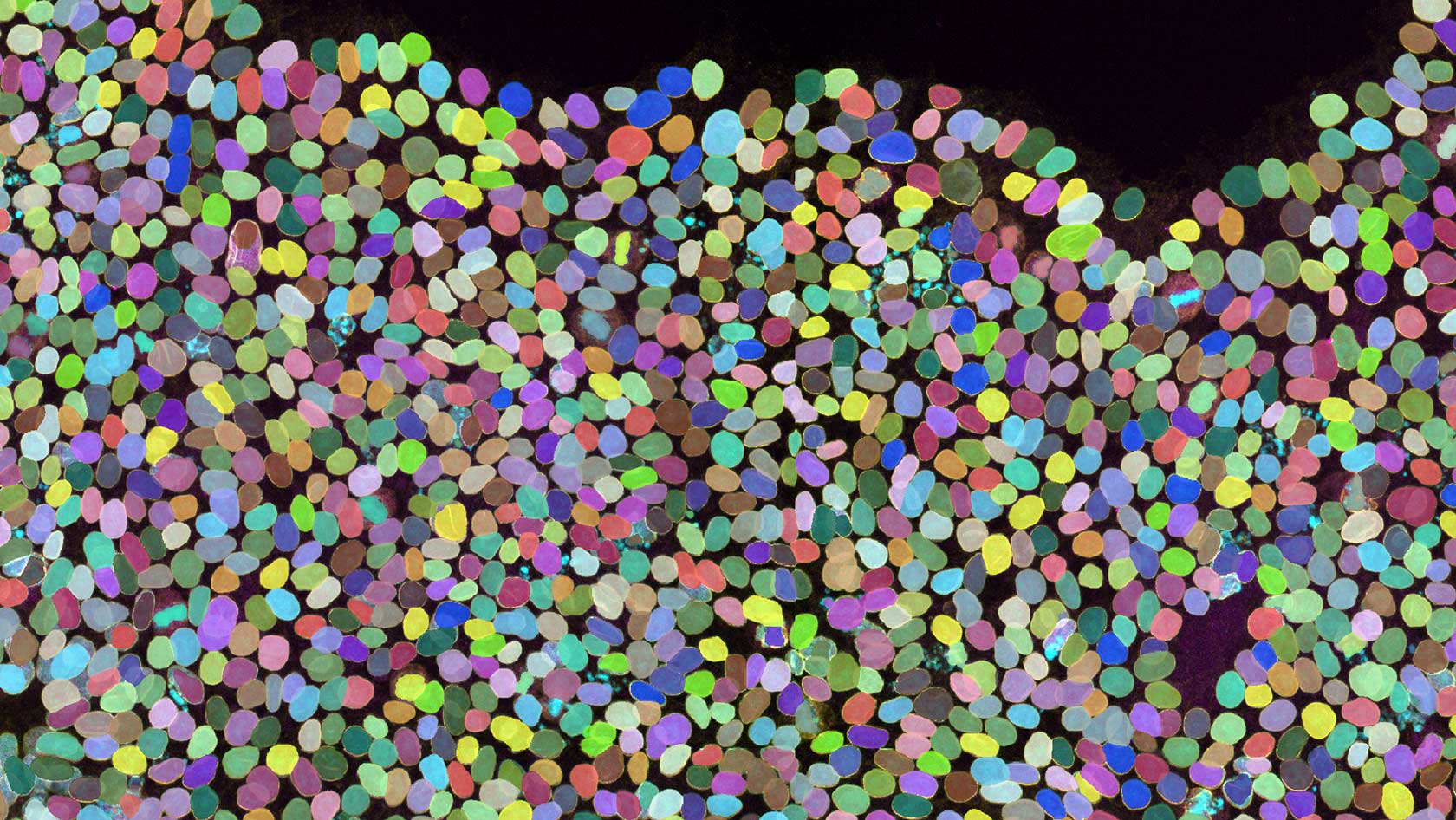
To conduct their investigations, Félix and her colleagues from the group led by Lucas Pelkmans, professor of systems biology, use tumor tissue taken directly from patients. In the lab, the cell samples are treated with a range of dye-labeled molecules that bind to specific proteins. Under the fluorescence microscope, it then becomes clear in which cells – and where in those cells – the tagged proteins accumulate. This is vital data, as the proteins either play a key role in tumor growth or indicate the type of tumor cell involved. The team can also test cancer drugs – around 50 at once – and track whether and how tumor cells respond to each. “This information can help tailor treatment to each patient’s specific tumor,” Pelkmans says.
Seeing a cell’s inner structure
Pelkman is based on Irchel Campus and specializes in microscopic methods. “By observing how cells and cell groups change during disease, we gain insights into where treatments are most likely to be effective,” he explains. Improving the efficiency of cancer treatment is also the mission of the Tumor Profiler Center, which Pelkmans co-founded. The center brings together research groups from the University of Zurich, ETH Zurich and University Hospital Basel, all working to harness biological imaging for personalized cancer therapy.

By observing how cells and cell groups change during disease, we gain insights into where treatments are most likely to be effective.
Humans have been studying living organisms for thousands of years in an effort to better understand them. “Throughout human history, visual observation has been the most important source of information about ourselves and our environment,” says Virginie Uhlmann, head of the BioVisionCenter, set up on the Irchel Campus in 2024 by UZH and the Friedrich Miescher Institute in Basel. Some of the earliest microscope images, dating to the early 17th century, were hand-drawn depictions of insects.
“Today, we have so many more possibilities,” Uhlmann says. Modern light microscopes achieve resolutions down to mere tenths of a micrometer – that’s ten-thousandths of a millimeter – enabling us to see the internal structure of living cells. For instance, we can see organelles such as the cell nucleus, mitochondria or protein clusters. And in the same way that microscopes have advanced, so have microscopic methods. One example is light sheet fluorescence microscopy, which can be used to track the development of large tissue samples over time by recording thin layers individually and then reconstructing them into a detailed 3D image. “At the same time, extracting so much information from these images has become much more complex,” the bioengineer says. “You can’t rely on the naked eye anymore.”
Research Spotlight: Why is Bioimaging so fascinating and how does it help us better understand diseases? (Video: Katharina Weins, Elvira Isenring MELS, UZH)
AI-driven image analysis
That’s why researchers now use algorithms – more and more often supported by AI – to detect and interpret structures in images. In the field of biological image analysis, this is known as “computer vision.” These methods allow researchers to obtain precise data from microscope images – such as the size of cells or organelles or the quantity of specific proteins. In principle, hundreds of different measurements can be taken from a single image, depending on the research question.
But because the images produced by different methods and instruments can vary widely, interpreting them is challenging, even when using AI. And most biologists aren’t experts in AI-supported image analysis, Uhlmann notes. “That’s why we need a bridge between biological microscopy and computer vision.” Building that bridge is the task assigned to her team at the BioVisionCenter.
“We’re working towards a future where researchers won’t need to find a new approach for every image type and research question,” Uhlmann says. “Instead, we’re developing file formats and processing tools that work for all kinds of images.” On her laptop, she opens a web platform called Fractal, a system her team is rapidly developing to make computer-assisted bioimage analysis accessible to everyone. The idea behind Fractal is to provide researchers with modular components that can be combined, enabling them to conduct analyses tailored to their specific research question. And thanks to its programming interfaces, other developers can integrate their own analysis tools into the platform too.
New levels of precision medicine
The first version of Fractal was developed by Lucas Pelkmans. Meanwhile, his group also now benefits from the upgraded platform to analyze microscopy images. The researchers have found that tumor cells respond to cancer drugs in highly diverse ways. Depending on a cell’s state and the connections within its complex signaling network, certain compounds can successfully block the cell cycle as intended – effectively putting the tumor cells on ice. However, if the same cells are in a different signaling state, entirely different drugs will work. “In some states, a drug might even speed up cell proliferation – the opposite of what you want,” Pelkmans says. “That has direct consequences for patient treatment.”
Personalized medicine – or, more accurately, precision medicine – already uses biological data from patients to tailor therapies as fittingly as possible. In oncology, for instance, genetic tests reveal which mutation caused a cancer. Based on this, about 10 tumor subgroups of skin, breast or lung cancer can now be identified and treated individually.
But as Pelkmans’ research and that of others has shown, treatment outcomes are even more predictable when we know and understand how a cell’s condition and molecular systems respond to different drugs. It’s precisely this kind of cellular context that can be made visible using imaging techniques – and across several orders of magnitude: from the details inside a single cell to multiple cells interacting within a tissue.
Unique tumors
“When you look at the cellular makeup, every tumor is unique – which is why they’re so hard to treat,” says Bernd Bodenmiller, professor of quantitative biomedicine and co-director of the Tumor Profiler Center. His team uses a different method to show what’s happening inside cells. At the Irchel Campus lab, Master’s student Jay Chang is measuring tissue from a biopsy sample provided by a cancer patient. He, too, is seated in front of a screen next to a large grey box – but instead of a microscope, it houses an imaging mass cytometer. This device uses mass spectrometry to detect antibodies labeled with isotopes, which are bound to specific proteins.
What makes it an imaging technique is the addition of a laser – a development in which Bodenmiller’s team played a leading role. In this method, a fine laser detaches a prepared sample – usually a thin slice of tumor tissue – and feeds it into the mass spectrometer in a predefined two-dimensional grid. Following this grid, the isotopes enter the mass spectrometer at precise intervals, allowing researchers to pinpoint exactly where each isotope-labeled protein was found: in which cell, on which organelle in that cell, and whether clustered with other proteins or separately.
As the researchers have 50 isotopes at their disposal, this method can be used to track up to 50 selected proteins simultaneously, revealing what different kinds of cells there are in a tumor, what’s happening inside the cells, and how they communicate. “This gives us a better understanding of the mechanisms that cause tumor cells to divide uncontrollably,” says Bodenmiller. Still other proteins can provide information about the immune cells in the tumor. “These immune cells are supposed to attack tumor cells, but sometimes they’re disactivated by certain proteins – which we can detect using imaging mass cytometry.”
Help for skin cancer patients
By enhancing the method to use specific peptides instead of isotopes to label the antibodies, Bodenmiller’s team was recently able to visualize over 120 proteins in tumor tissue at once. “We’ll soon be able to track even more,” he says. The more proteins researchers can visualize inside cells, the clearer the picture of what’s happening becomes – and the more precise the therapy recommendations.
All these imaging methods for precision medicine come together at the Tumor Profiler Center, where they’re already benefiting patients. In a first clinical study, the approach was tested on skin cancer patients for whom standard diagnostics and treatments no longer worked. For these patients, biological imaging provided critical information for targeted follow-up therapies – with success. According to early results, patients who received the treatment lived longer than those without the benefit of imaging data. Some were still alive two years later, which is rarely the case with skin cancer at such an advanced stage.
“So we now know that biological imaging truly improves treatment,” Pelkmans says. However, larger clinical trials are still needed to ensure these approaches reach more patients. Some methods also need to be faster and more cost-effective for clinical use. Spin-off companies founded by participating research groups are already working on this. One thing is clear, as Pelkmans states: “With biological imaging, we have the potential to make medicine significantly more targeted and personalized.”