When Resistant Germs Travel
What can happen to humans can happen to animals as well. They’re admitted to hospital and receive treatment, but when they get back home, they may be carrying some unwanted guests – bacteria that are resistant to antibiotics. This resistance can be transmitted to humans who come into close contact with animals. The veterinarian Barbara Willi was able to demonstrate how this happens. The attending physician specializes in clinical infectious diseases at the Clinic for Small Animal Internal Medicine at the Veterinary Teaching Hospital of the University of Zurich. Working closely with fellow researchers at the University of Bern, Willi investigated the role of small animal clinics when it comes to spreading bacteria that are resistant to antibiotics. “We found poor hygiene standards in several clinics, and many were heavily contaminated with resistant germs,” explains the veterinarian.
In one of the clinics, the situation was particularly alarming. The researchers found highly resistant bacteria in more than 20 percent of the cats and dogs treated there. Only one of the furry patients had these bacteria before entering the clinic. “In all other cases, the animals had acquired the resistant bacteria in the clinic,” says Barbara Willi. The most important means of transmitting resistant bacteria are the hands of clinic staff. As Willi’s research revealed, hand hygiene in all of the clinics included in the study was poor.
Antibiotic resistance picked up in clinics can also become a problem for the animals’ owners, as Barbara Willi showed in a different study, in which she traced two dogs after they had received veterinary care in a clinic. In both cases, the resistant germs were transmitted from the dogs to their owners. Rather alarmingly, one of the canines carried the germs for over two months, and the bacteria were found in 24 percent of swabs and samples collected throughout the household. “Our studies reveal that animal clinics may play an active role when it comes to spreading multidrug-resistant organisms,” concludes the infectious diseases expert.
Healthy through and through
“If we want to fight these resistant bacteria effectively, we have to know everything about the ways in which they spread,” says Roger Stephan, professor of veterinary food safety and hygiene and dean of the Vetsuisse Faculty at UZH. Since resistant bacteria occur in humans, animals and the environment alike, Stephan believes they should be explored using the One Health approach, which covers all three dimensions and, crucially, the areas where they overlap. One Health is based on an understanding that the health of people is intertwined with the health of animals and our shared environment. People and animals need a healthy environment to be able to stay well; people need healthy animals and vice versa. This of course implies that people can make animals sick, and the other way round.
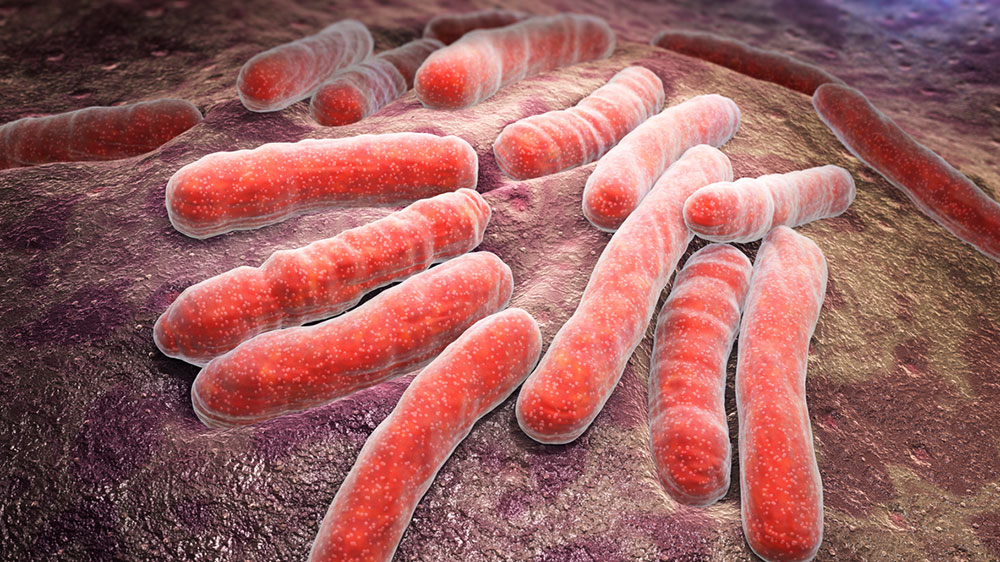
Combating antibiotic resistance is at the very top of the One Health agenda. Antibiotics are still one of the most important weapons when it comes to treating bacterial infections. With the selection and spread of resistant bacteria, this weapon loses much of its power. Scientists have thus been warning that we’re entering a post-antibiotic era, a time when many infectious diseases that can currently be treated successfully if diagnosed in time will go back to being deadly.
Despite the availability of antibiotics, infectious diseases such as pneumonia, diarrheal diseases and tuberculosis are still among the most common causes of death worldwide, accounting for around one in three deaths. Fatal bacterial infections are becoming an increasingly serious issue in developed countries, too. In Europe, for example, healthcare-associated (or nosocomial) infections are on the rise – infectious diseases that are acquired in hospitals or healthcare facilities.
Resistant bacteria in water and manure
This is also due to antibiotic-resistant germs, which in a hospital environment have ideal conditions to thrive (see box). And there’s almost nothing we can do about this, since they’re often multiresistant and can only be treated with a small number of “reserve” antibiotics. These antibiotics – fittingly also known as drugs of last resort – could be described as the “nuclear option” for fending off infections, and as such they’re only used after all other options have failed to produce an adequate response in the patient. Even so, resistance to these last-resort antibiotics is already developing.
In addition to the direct transmission pathways, bacteria are also finding other, more intricate ways of reaching new hosts and spreading their antibiotic-resistant genes. The most popular of these paths include water and manure. When resistant bacteria are released into the sewer system by humans and animals, wastewater treatment facilities often fail to remove all of the bacteria from the sewage. Veterinary scientist Roger Stephan has explored the implications of this across several studies. “There is an alarming number of resistant bacteria in our rivers and lakes,” says Stephan. The further down a river you go, the more likely you are to find traces of resistant bacteria.
So if you fancy a swim in the Rhine river, you’re better off doing so in Chur than in Basel, and it’s probably best to avoid going in the water altogether once the river reaches Cologne. Stephan has also discovered another transmission route: “In summer, our fields are increasingly irrigated with water from rivers,” he explains, “and that’s how the bacteria end up on plant-based produce. The plants can absorb the bacteria through their roots.” And once they’re inside the plants, even the most thorough scrubbing and rubbing won’t help – so in addition to the vitamins and nutrients in our salad, we may unwittingly also be consuming antibiotic-resistant bacteria.
Another way these bacteria are released into the environment is through manure. Xaver Sidler, professor of swine medicine at UZH, explored this particular transmission pathway in a study by fertilizing clover and spring wheat with pig manure. After three weeks, the researcher found resistant germs in the soil as well as on the plants. Clover is often used as fodder, while wheat is made into flour. “The resistant bacteria are destroyed during the baking process,” says Xaver Sidler, offering at least some good news. And this bright spot is much needed, as talking about the topic with veterinary scientists can make you feel as if resistant germs have spread all over, with almost nothing standing in their way.
Policy-makers have also started taking an interest in stopping the spread of antibiotics resistance, for example with the Swiss Antibiotic Resistance Strategy (StAR) adopted by the Federal Council in 2015. The strategy includes the following words: “We cannot stop bacteria becoming resistant to antibiotics, but we are all responsible for ensuring that this natural process of adaptation is not encouraged.”
Use of antibiotics cut in half
So what specific action can we take to curb the bacteria’s “natural” selection process? In other words, how can we stop them from becoming resistant? Veterinarians and physicians agree that moderate use of antibiotics is key – in human as well as veterinary medicine. Antibiotics are especially problematic when it comes to animals that are used for food. “The use of antibiotics in pig farming was able to be cut more than in half over the past 10 years,” says Xaver Sidler. How was this achieved? “The most important thing is for the animals not to get sick in the first place,” explains Dolf Kümmerlen, attending physician at the Veterinary Teaching Hospital’s Division of Swine Medicine. Veterinarians have developed a corresponding concept and made recommendations based on four pillars: Recognizing risk factors, improving hygiene in pigsties, creating an ideal environment for animals, and preventing germs getting in from outside.
When it comes to hygiene, for example, this means cleaning out the sty before new pigs are introduced. An ideal environment refers to having the right temperature and avoiding drafts and harmful gases. This matters, because pigs are prone to developing respiratory or diarrheal diseases. Thirdly, as few germs as possible should be carried into the sty from the outside, for example by animal carers, new animals, mice and rats, insects, or through the food and water.
Improved hygiene and husbandry reduces the infection pressure. The animals’ resilience can be increased by taking additional measures, emphasizes Xaver Sidler, for example by adopting breeding goals that take into account the health of the animals, or preventive action such as vaccination.
No licking!
Another important initiative supported by UZH veterinarians is the monitoring of antibiotics use, where farmers disclose in a database how many antibiotics they are using for which diseases. “Each farmer then knows where they stand compared to others,” explains Dolf Kümmerlen, “and this encourages the farmers to use antibiotics as sparingly as possible.” The monitoring also provides crucial data for researchers, and it exposes farms that are still using large quantities of antibiotics. All things considered, pig farmers have already taken significant strides in curbing antibiotic resistance. “But there is still a lot of untapped potential, and a lot of work still needs to be done,” says Xaver Sidler. It’s clear that the use of antibiotics in animal husbandry is more than merely a health issue. For the farmers, it is also a matter of reputation, which could end up threatening their livelihood. After all, who wants to eat food that’s contaminated with resistant germs?
What goes for farmers also applies to animal clinics, of course – hygiene must improve. “The hygiene concepts in place are actually very good,” says Barbara Willi, “but they also have to be put into practice.” Predictably yet crucially, this includes good hand hygiene. “People often forget about this, especially before touching animal patients or performing tasks such as taking blood samples or puncturing a vein.” Animals carrying resistant bacteria should be isolated and treated in clinics by vets wearing protective clothing. Of course, owners of small pets should also make sure hygiene is maintained. “Cats and dogs shouldn’t lick people or sleep in the same bed as their owners. Hands need to be washed after every contact,” recommends Barbara Willi. While this isn’t always easy to do in everyday life, these rules should be strictly followed nevertheless. After all, our pets may not only transmit antibiotic-resistant germs, but other pathogens as well.