Broadly neutralizing HIV antibodies pave the way for vaccine
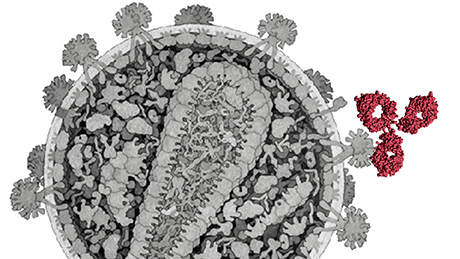
We know from HIV research that around one percent of people infected with HIV form antibodies that combat different virus strains. These broadly neutralizing HIV antibodies (bnAbs) bind to structures on the surface of the virus which barely change and are identical in different viral strains. Dubbed “spikes”, these sugar and protein complexes are the only surface structures that stem from the HIV virus itself and can be attacked by the immune system via antibodies. Due to their broad impact, these antibodies constitute a promising cornerstone for the development of an effective vaccine against HIV.
Virus load, virus diversity and duration of infection encourage antibody formation
A Switzerland-wide team of researchers headed by the University of Zurich and University Hospital Zurich conducted an extensive study on the factors responsible for the formation of broadly neutralizing antibodies against HIV. They examined around 4,500 people infected with HIV who are recorded in the Swiss HIV Cohort Study and the Zurich Primary HIV Infection Study, and identified 239 people who form such antibodies.
Firstly, three disease-specific characteristics are important: the number of viruses present in the body, the diversity of the virus types found and the duration of an untreated HIV infection. “Our study enabled us to show for the first time that each of these three parameters – virus load, virus diversity and infection duration – influences the development of broadly neutralizing antibodies independently of each other,” explains Huldrych Günthard, professor of clinical infectious diseases at UZH. “So we don’t necessarily have to consider all three parameters in designing an HIV vaccine. This is especially important with regard to the length of vaccine administration – it wouldn’t be possible to imitate a longer untreated HIV infection with a vaccine.”
Black people form broadly neutralizing HIV antibodies more frequently
A second factor concerns ethnicity: Black HIV patients form broadly neutralizing antibodies more frequently than white people – irrespective of the other factors analyzed in the study. For Alexandra Trkola, a professor of medical virology at UZH, this surprising discovery needs to be studied more closely: “First of all, we need to understand more precisely what significance and impact the genetic, geographical and socio-economic factors of people from different ethnicities have on the formation of these antibodies.”
Different virus sub-types influence the antibodies’ binding site
The third factor involves the influence of the virus sub-type on antibody formation. While the frequency of the antibody production remains unaffected, the researchers showed that the virus sub-type has a strong influence on the antibody type formed. Sub-type B HIV viruses are more likely to lead to the production of antibodies directed against the region of the virus surface through which it binds to human immune cells (CD4 binding site). By contrast, non sub-type B virus favor the production of antibodies which bind to a sugar element of the virus spikes (V2 glycan). Specific structural features on the virus shell thus affect the antibodies’ binding specificity depending on the virus sub-type.
“Our results show how different factors boost the formation of antibodies that broadly combat different viral strains,” concludes Trkola. “This will pave the way for us to systematically push ahead with the development of an effective vaccine against HIV.”
Literature:
Peter Rusert, Roger D. Kouyos, Claus Kadelka, Hanna Ebner, Merle Schanz, Michael Huber, Dominique L. Braun, Nathanael Hozé, Alexandra Scherrer, Carsten Magnus, Jacqueline Weber, Therese Uhr, Valentina Cippa, Christian W. Thorball, Herbert Kuster, Matthias Cavassini, Enos Bernasconi, Matthias Hoffmann, Alexandra Calmy, Manuel Battegay, Andri Rauch, Sabine Yerly, Vincent Aubert, Thomas Klimkait, Jürg Böni, Jacques Fellay, Roland R. Regoes, Huldrych F. Günthard, Alexandra Trkola and the Swiss HIV Cohort Study. Determinants of HIV-1 broadly neutralizing antibody induction. Nature Medicine. September 26, 2016. doi:10.1038/nm.4187