Heinrich B. was seriously ill. His diagnosis: melanoma. The 41-year-old accountant had already been told of multiple metastases in his skin when a computer tomography conducted in 2017 detected offshoots in his lungs too. Hopes were raised by a course of antibody-based immunotherapy, only to be dashed again by a relapse when new metastases appeared. The active cyclist suffered badly from his physical weakness. More sessions of chemotherapy and immunotherapy were unsuccessful. With all therapy options for Heinrich B. exhausted, his doctor no longer knew how to proceed.
Melanoma is the most malignant form of all skin cancers and the fifth most common cancer in Switzerland. About 3,000 people are diagnosed with the condition every year, men and women being equally affected. 62-year-old teacher Sabine M. was also struggling with a metastatic melanoma. Having remained undetected for so long, the cancer was able to dig into deeper layers of her skin, spread through her body’s blood and lymph channels and form its metastases. In such cases, treatment is difficult. The disease had such an impact on her health that the dedicated German teacher could no longer supervise her class through to their Matura exams. She told a friend: “I’m metastasized through and through.” She coined the phrase herself, evidence of her desperation.
Every cancer is different
Although Heinrich B. and Sabine M. were both diagnosed with skin cancer, every cancer is different. Traditionally, cancers have always been described using the name of the organ where they first occur, such as skin, breast or bowel cancer. “But we now know that this is not only an outdated view of things, but also one that is not entirely correct,” says Andreas Wicki, professor of oncology at UZH and senior consultant physician at the UniversityHospital Zurich where he is deputy director of the Department of Medical Oncology and Haematology Clinic. Tumors that originate in different organs, for example, can actually be more similar to one another in biological terms than different types of tumors from the same organ. Currently, about 200 various cancer diseases are known. For many of these cancers, research conducted over recent years has managed to identify the genetic alterations specifically responsible for the tumors. But differences can occur even in the same patient. “This is when metastases differ genetically from the primary tumor,” Wicki explains.
On a molecular basis, therefore, each cancer is unique and characterized by the combination of its mutations. If these differences can be taken into account when oncologists consider treatment, therapies that generate only adverse side effects and no medical benefit can be omitted. Conversely, the risk of failing to prescribe a promising therapy decreases.
Personally tailored treatments
For Sabine M. and Heinrich B., a new opportunity arose three years ago when they heard about a study forming part of the Tumor Profiler project. In this study, the Tumor Profiler team vowed to analyze the cancer of each individual patient right down to the cellular and molecular level, with the aim of using the analyses to deliver promising therapy recommendations to the patient’s oncologist as rapidly as possible. This could result in new alternatives also for patients like Sabine M. and Heinrich B. who had already exhausted all existing therapy options. Both cancer patients decided to take part in the study. Led by Andreas Wicki, it started with 240 patients, 95 of whom suffered from metastatic melanoma and the rest from metastatic ovarian cancer or acute myeloid leukemia.
Once samples had been taken from biopsies on the study participants, including Heinrich B. and Sabine M., it was important that the sensitive cells were sent to the seven participating laboratories as quickly as possible (see box); more than a hundred researchers then had about two weeks to evaluate the samples. This was a major logistical challenge, as each of the seven specialized laboratories focused on one specific method. Within the scope of testing, factors being examined included DNA, RNA, proteins in the cancer cells, and cells in the immune system. “What is new and revolutionary about our approach is our combination of analytical methods and our data processing pipeline,” Wicki says.
This is how samples from Heinrich B. and Sabine M. reached the laboratory run by Lucas Pelkmans, professor of molecular biology at UZH. He is responsible for carrying out in vitro drug tests. In Switzerland there are about 180 cancer drugs approved by Swissmedic, about 60 of which are regularly used in cancer treatments. The researchers work with known drugs or with a new mix of drugs and test ex vivo how the tumor cells of cancer patients react to them. The aim is to understand which processes in the cell are influenced by which drugs and whether certain drugs, which have not previously been used for the specific type of cancer under examination, work in the specific sample. This is how new treatment options are created. One result from the tests: in certain cases it may be better to use drugs that are approved for other types of cancer than to work with the standard therapy.
Understanding the tumor
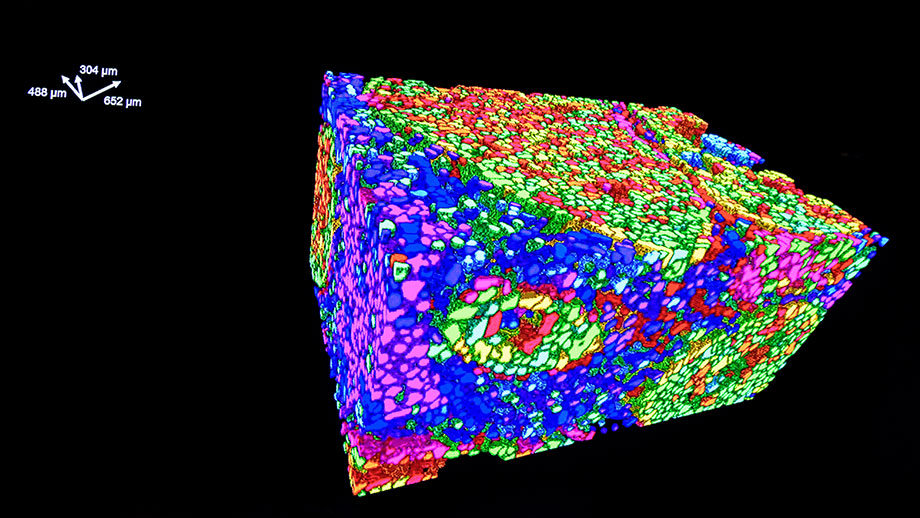
In another laboratory, UZH professor Bernd Bodenmiller and his team also analyzed Heinrich B. and Sabine M.’s tissue samples. “We’ve succeeded in developing a unique method that enables us to visualize dozens of biomarkers in the tissue simultaneously,” says Bodenmiller, director of the Department of Quantitative Biomedicine at UZH and professor in the Department of Biology at ETH Zurich. “We look at the immune cells and the tumor cells and see how they act in spatial terms and how they potentially communicate.” The biomarkers give the researchers a picture of the state of the tumor. “We recognize the components of a tumor and how they interact. This allows us to target and disrupt its function with the use of drugs.”
The last links in the chain are the Leonhard Med Secure Scientific Platform Service and Nexus Personalized Health Technologies at ETH Zurich. Here, the data from the seven laboratories are compiled and analyzed with the help of data specialists and algorithms. The ETH data scientists compile the data for the interdisciplinary tumor board. Afterwards, the treating oncologists discuss the new treatment with their patients. “We’ve developed an advancement in oncology, one that serves the patients,” says Mitch Levesque, UZH professor of experimental skin cancer research, one of the researchers involved in the study.

Good News
The work conducted by the Tumor Profiler team was able to help Heinrich B. and Sabine M. too. A few weeks after his biopsy, Heinrich B. received a new immunotherapy based on the laboratories’ analyses – and over the next few months, his tumor shrank. It was the same story with Sabine M., who was given a new immunotherapy in combination with a kinase inhibitor: drugs that bind specific enzymes and inhibit their function. For some of the patients in the study with melanoma, the researchers were able to draw a surprisingly positive conclusion: “We were able to help a third of the cancer patients who’d exhausted all other options by prescribing an individually tailored mix of drugs based on their tumor profiler analysis. Their tumors shrank,” Andreas Wicki reports. “And in more than half of the participants, the tumor growth could at least be stabilized.” A success story – Heinrich B. and Sabine M., at least, are happy. Heinrich B. can ride his bike long distances again and Sabine M. is back teaching at school, albeit on a reduced schedule.