Navigation auf uzh.ch
Navigation auf uzh.ch
Neurodegenerative diseases cause some of the neurons in our brains to die, resulting in different symptoms depending on the brain region affected. In amyotrophic lateral sclerosis (ALS), neurons in the motor cortex and spinal cord degenerate, leading to paralysis. In frontotemporal dementia (FTD), on the other hand, neurons located in the parts of the brain involved in cognition, language and personality are affected.
Both ALS and FTD are relentlessly progressive diseases and effective treatments are still lacking. As the population ages, the prevalence of age-related neurodegenerative diseases such as ALS and FTD is expected to increase.
Despite the identification of the aberrant accumulation of a protein called TDP-43 in neurons in the central nervous system as a common factor in the vast majority of ALS and about half of FTD patients, the underlying cellular mechanisms driving neurodegeneration remain largely unknown.
In their study, first author Marian Hruska-Plochan and corresponding author Magdalini Polymenidou of the Department of Quantitative Biomedicine at the University of Zurich developed a novel neural cell culture model that replicates the aberrant behavior of TDP-43 in neurons. Using this model, they discovered a toxic increase in the protein NPTX2, suggesting it as a potential therapeutic target for ALS and FTD.
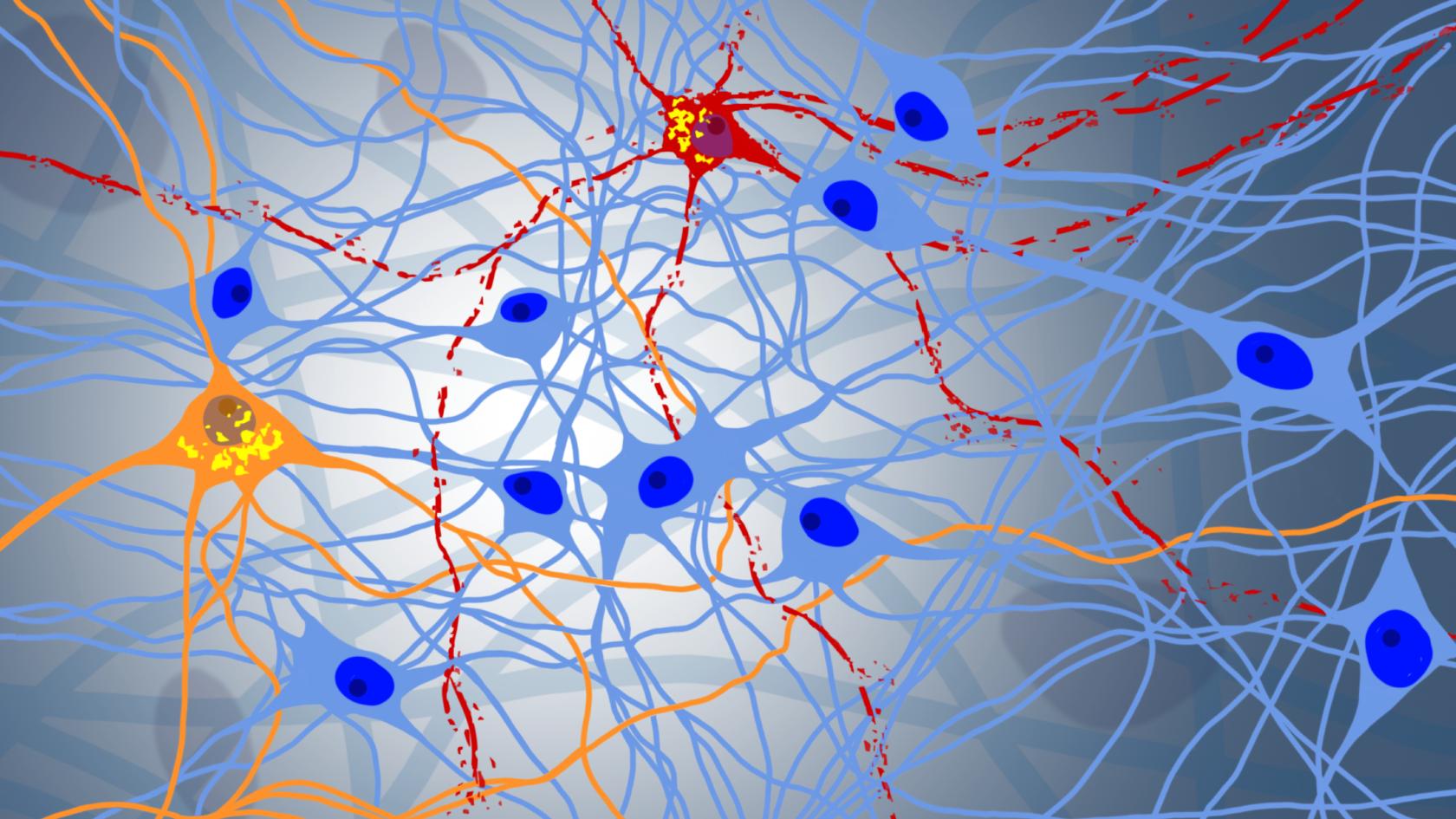
To mimic neurodegeneration, Marian Hruska-Plochan developed a new cell culture model called “iNets” (shortened from “interconnected neuronal networks”), derived from human induced pluripotent stem cells. These cells, originated from skin cells and reprogrammed to a very early, undifferentiated stage in the laboratory, serve as a source for developing many different, desired cell types. iNets are a network of interconnected neurons and their supporting cells growing in multiple layers in a dish.
The cultures lasted exceptionally long – up to a year – and were easily reproduced. “The robustness of aging iNets allows us to perform experiments that would not have been possible otherwise,” says Hruska-Plochan. “And the flexibility of the model makes it suitable for a wide range of experimental methodologies.” As a case in point, the iNets cell cultures provided the ideal model to investigate the progression from TDP-43 dysfunction to neurodegeneration.
Employing the iNets model, the researchers identified a toxic accumulation of NPTX2, a protein normally secreted by neurons through synapses, as the missing link between TDP-43 misbehavior and neuronal death. To validate their hypothesis, they examined brain tissue from deceased ALS and FTD patients and indeed found that, also in patients, NPTX2 accumulated in cells containing abnormal TDP-43. This means that the iNets culture model accurately predicted ALS and FTD patient pathology.
In additional experiments in the iNets model, the researchers tested whether NPTX2 could be a target for drug design to treat ALS and FTD. The team engineered a setup in which they lowered the levels of NPTX2 while neurons were suffering from TDP-43 misbehavior. They found that keeping NPTX2 levels low counteracted neurodegeneration in the iNets neurons. Therefore, drugs that reduce the amount of the protein NPTX2 have potential as a therapeutic strategy to halt neurodegeneration in ALS and FTD patients.
Magdalini Polymenidou sees great promise in this discovery: “We still have a long way to go before we can bring this to the patients, but the discovery of NPTX2 gives us a clear shot of developing a therapeutic that acts at the core of the disease,” she said. “In conjunction with two additional targets recently identified by other research teams, it is conceivable that anti-NPTX2 agents could emerge as a key component of combination therapies for ALS and FTD in the future,” she added.
Marian Hruska-Plochan, Vera I. Wiersma, Katharina M. Betz, et al., Magdalini Polymenidou. A model of human neural networks reveals NPTX2 pathology in ALS and FTLD. Nature (2024). DOI: 10.1038/s41586-024-07042-7